ICD 10 Hyperlipidemia: Complete Guide for Better Understanding

Explore everything about ICD 10 hyperlipidemia, including its coding details, causes, types, treatment options, and FAQs. A complete expert-written guide for healthcare professionals and patients.
Introduction to ICD 10 Hyperlipidemia
When it comes to understanding medical conditions, one of the most important aspects is knowing how they are classified and coded. That’s where the ICD 10 hyperlipidemia code becomes highly relevant. This code is used worldwide in medical records, insurance claims, and healthcare systems to track and categorize cases of hyperlipidemia. Hyperlipidemia itself refers to the presence of high levels of lipids or fats in the blood, which can include cholesterol and triglycerides. These elevated levels are often silent, meaning a person may not experience noticeable symptoms until complications arise, such as heart disease or stroke.
The ICD 10 system, short for the International Classification of Diseases, Tenth Revision, is a universal coding system managed by the World Health Organization. Within this framework, hyperlipidemia has a dedicated code that makes it easier for physicians, researchers, and billing departments to communicate efficiently. Having a proper code assigned to a condition like hyperlipidemia helps in standardizing diagnosis, ensuring accurate patient records, and improving public health statistics.
Understanding Hyperlipidemia
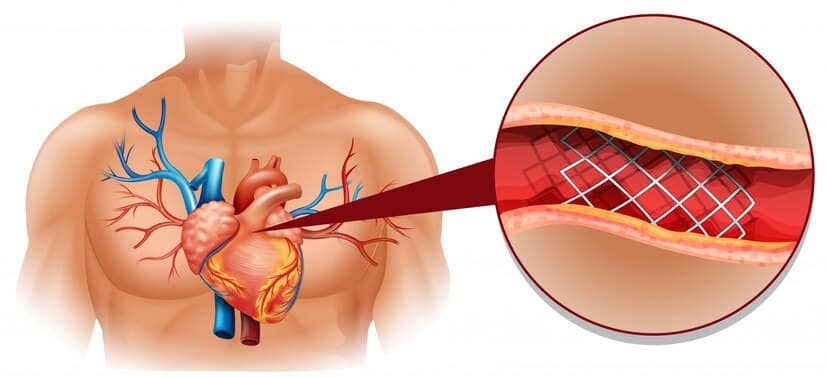
Hyperlipidemia might sound like a complex term, but at its core, it’s simply a condition involving abnormal lipid levels in the blood. Lipids are fats, and while the body needs a certain amount for energy and cell function, too much can pose serious risks. Elevated lipid levels, especially cholesterol and triglycerides, contribute to the buildup of fatty deposits in blood vessels. Over time, this buildup restricts blood flow and increases the risk of cardiovascular events.
It’s important to note that hyperlipidemia is not a disease on its own but rather a risk factor for several other health problems. For example, coronary artery disease, hypertension, and metabolic syndrome are often linked with poorly controlled lipid levels. Many people are unaware they have hyperlipidemia until they undergo routine blood tests, which makes screening and awareness crucial.
What is ICD 10 Hyperlipidemia?
In simple terms, ICD 10 hyperlipidemia refers to the diagnostic code that medical professionals use to represent hyperlipidemia in patient charts. The ICD 10 code for unspecified hyperlipidemia is E78.5. This particular code is applied when a doctor diagnoses a patient with high lipid levels but does not specify the exact type, such as whether it involves high cholesterol, high triglycerides, or both.
Having a standard code like E78.5 ensures that hyperlipidemia is documented consistently across hospitals, clinics, and insurance databases. This is vital for multiple reasons. First, it helps with patient care by allowing continuity when different healthcare providers review the same records. Second, it ensures billing accuracy, which is a major factor in insurance reimbursements. Finally, it supports research by enabling large-scale data collection, which helps scientists study trends and develop better treatments.
Types of Hyperlipidemia
Hyperlipidemia can be categorized into different types depending on which lipids are elevated. The ICD 10 coding system includes specific codes for these variations, making it easier to distinguish between them in medical records.
One common type is familial hyperlipidemia, which is inherited genetically. This condition often leads to significantly high cholesterol levels at an early age, increasing the risk of premature heart disease. Another type is secondary hyperlipidemia, which develops due to other conditions such as diabetes, obesity, or hypothyroidism. Identifying the underlying type is critical because it influences the treatment plan.
For example, if high triglycerides are the main issue, lifestyle interventions like reducing sugar and alcohol intake may be emphasized. In contrast, if high LDL cholesterol is the problem, statin therapy might be the first choice. The ICD 10 system recognizes these distinctions by assigning more precise codes when possible, although E78.5 remains the umbrella term for unspecified cases.
Causes of Hyperlipidemia
The causes of hyperlipidemia can be broadly classified into two categories: genetic and lifestyle-related. Genetic causes include familial hypercholesterolemia, which runs in families and leads to dangerously high cholesterol levels regardless of diet. People with genetic forms of hyperlipidemia often require medication early in life to reduce their risk of heart problems.
On the other hand, lifestyle factors play a massive role in secondary hyperlipidemia. A diet high in saturated fats, trans fats, and processed sugars can significantly elevate lipid levels. Lack of physical activity, smoking, and excessive alcohol consumption also contribute to the condition. Additionally, medical conditions like diabetes, kidney disease, and thyroid disorders can act as secondary causes. Understanding these factors helps both doctors and patients take proactive steps to manage the condition effectively.
Symptoms and Diagnosis
One of the challenging aspects of hyperlipidemia is that it usually doesn’t cause obvious symptoms. Most people discover they have high cholesterol or triglycerides during routine blood work. In rare cases, very high lipid levels can lead to visible signs such as fatty deposits under the skin, known as xanthomas. However, these are uncommon and typically occur in genetic forms of the condition.
Diagnosis involves a simple blood test called a lipid panel. This test measures total cholesterol, LDL cholesterol (often called “bad” cholesterol), HDL cholesterol (known as “good” cholesterol), and triglycerides. Doctors use these values to assess cardiovascular risk and decide on the best management approach. The results are then recorded in the patient’s chart using the ICD 10 hyperlipidemia code, ensuring proper documentation.
ICD 10 Hyperlipidemia in Medical Records
The importance of coding cannot be overstated in modern healthcare. Using the ICD 10 hyperlipidemia code ensures that the diagnosis is officially documented and communicated effectively across different systems. This is particularly important in large hospitals where multiple specialists may be involved in a patient’s care.
For example, a cardiologist treating a patient with heart disease needs to know if hyperlipidemia has already been diagnosed by the primary care provider. By reviewing the ICD 10 coding in the patient’s electronic health record, they can immediately access that information without needing repeated tests. Similarly, insurance companies rely on these codes to process claims accurately. Without proper coding, reimbursement delays and administrative issues could arise.
Treatment Options for Hyperlipidemia
Managing hyperlipidemia typically involves a combination of lifestyle changes and medication. Lifestyle modifications are the foundation of treatment. These include eating a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins while reducing intake of saturated fats and processed foods. Regular exercise is equally important, as physical activity helps raise HDL cholesterol and lower triglycerides.
For many patients, lifestyle changes alone may not be enough, particularly if they have genetic forms of hyperlipidemia. In such cases, medications like statins are prescribed to lower LDL cholesterol. Other options include fibrates, niacin, and omega-3 fatty acid supplements for high triglycerides. The ICD 10 hyperlipidemia code allows doctors to track the effectiveness of these treatments over time by monitoring outcomes within electronic health systems.
The Role of Prevention
Prevention plays a key role in reducing the burden of hyperlipidemia on both individuals and healthcare systems. Simple steps like maintaining a balanced diet, staying active, avoiding smoking, and keeping a healthy weight can drastically lower the risk of developing high lipid levels. Regular check-ups are also important, as they allow for early detection and intervention.
Healthcare providers often encourage patients to know their numbers—meaning their cholesterol and triglyceride levels—so they can take action before complications develop. Since ICD 10 coding is used for statistical analysis, prevention programs benefit by understanding how common hyperlipidemia is in different populations. This information helps governments and health organizations plan effective strategies.
ICD 10 Hyperlipidemia and Public Health
From a public health perspective, ICD 10 hyperlipidemia coding is more than just a technical detail. It provides valuable data that helps track the prevalence of high lipid levels across regions and demographics. This information is essential for developing policies aimed at reducing cardiovascular disease, which remains the leading cause of death worldwide.
By analyzing coding data, researchers can identify trends, such as whether certain age groups or communities are at higher risk. This allows for targeted education campaigns and preventive efforts. For instance, if a particular population shows high rates of hyperlipidemia, health agencies can focus resources on screening programs and awareness initiatives in that area.
Common Myths About Hyperlipidemia
There are several myths surrounding hyperlipidemia that need to be cleared up. One common misconception is that only overweight individuals can have high cholesterol. In reality, even people with a normal weight can develop hyperlipidemia due to genetics or other medical conditions.
Another myth is that once you start medication like statins, you can stop worrying about diet and exercise. This is far from true. Medications are highly effective, but they work best when combined with healthy lifestyle habits. The ICD 10 hyperlipidemia code is a reminder that proper management is ongoing and requires both medical treatment and lifestyle commitment.
Table: Lipid Categories and Their Risks
| Lipid Type | Normal Range (mg/dL) | Risk if Elevated |
|---|---|---|
| Total Cholesterol | < 200 | Heart disease, stroke |
| LDL (“Bad”) | < 100 | Atherosclerosis, heart attack |
| HDL (“Good”) | > 60 | Low HDL raises risk |
| Triglycerides | < 150 | Pancreatitis, cardiovascular risk |
FAQs on ICD 10 Hyperlipidemia
What is the ICD 10 code for hyperlipidemia?
The ICD 10 code for unspecified hyperlipidemia is E78.5. It is used when the type of lipid abnormality is not specified in the diagnosis.
Is hyperlipidemia the same as high cholesterol?
Not exactly. Hyperlipidemia includes both high cholesterol and high triglycerides. High cholesterol is one type of hyperlipidemia.
Can hyperlipidemia be cured?
It can be managed effectively with lifestyle changes and medications, but genetic forms may require lifelong treatment. Cure is not always possible, but control is achievable.
Why is ICD 10 coding important for hyperlipidemia?
It ensures accurate medical documentation, facilitates insurance billing, and provides essential data for research and public health planning.
Does everyone with hyperlipidemia need medication?
Not always. Some people can manage it with diet and exercise alone, while others, especially those with genetic forms, will require medication.
Can children have hyperlipidemia?
Yes, particularly if it is inherited. Children with familial hyperlipidemia need early screening and treatment to reduce long-term risks.
Conclusion
Hyperlipidemia is a silent yet significant health condition that affects millions of people worldwide. By using the ICD 10 hyperlipidemia code, healthcare providers ensure consistent diagnosis, better communication, and accurate record-keeping. While the condition often goes unnoticed until complications arise, routine screening, healthy living, and proper treatment can make a world of difference. Ultimately, understanding this condition and its coding is not just about medical paperwork—it’s about improving health outcomes for individuals and communities alike.